
– Key features of femoral artery anatomy
The common femoral artery (CFA) is the prolongation of the external iliac artery and begins midway behind the inguinal ligament (which is directed from the anterior superior spine of the ilium to the symphysis pubis). For the interventionalist, an important vascular-anatomic marker of the relationship between external iliac, CFA and inguinal ligament is represented by the inferior epigastric artery which arises from the external iliac artery immediately above the inguinal ligament, initially descends without crossing it and soon ascends to the abdominal wall crossing the ligament at the lowest point of its course. (FIGURE 1)
In the upper third of the thigh, the CFA lies, in front of the hip joint, in the femoral (or Scarpa’s) triangle. The artery is enclosed for the first 4 cm, laterally to the femoral vein and medially to the femoral nerve. The important relationships of these structures may be easily remembered by the “NAVY” mnemonic acronym (Nerve, Artery, Vein, emptY space). (FIGURE 1)
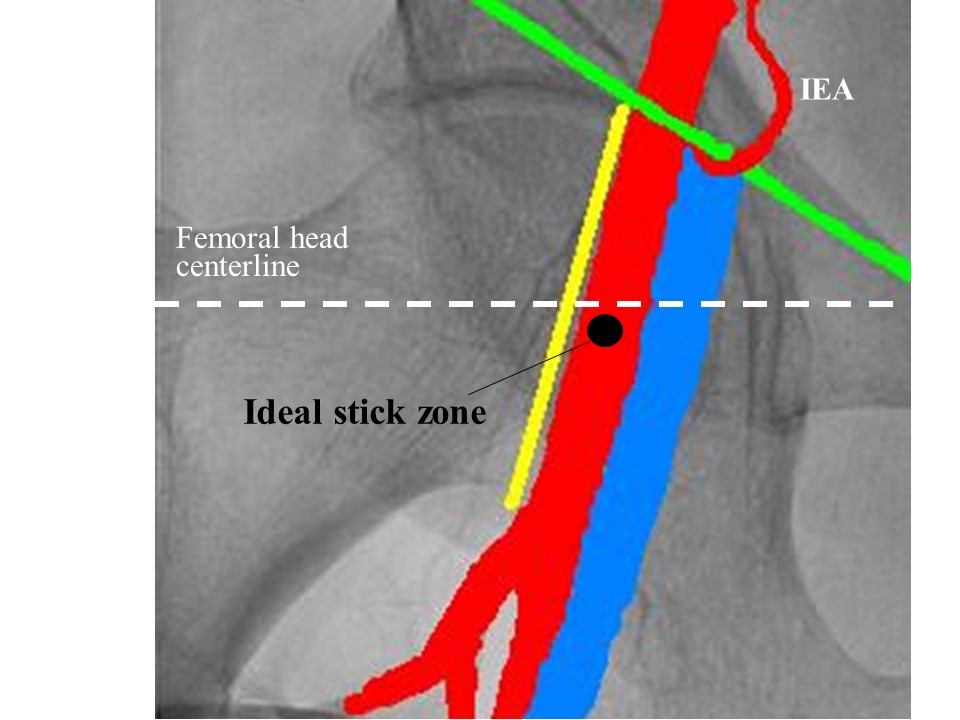
Figure 1
The femoral vessels run from the middle of the base to the apex of the femoral triangle. In its course the CFA gives many (small) lateral branches and, from 2 to 5 cm below the inguinal ligament, divides into the femoral bifurcation vessels, the superficial femoral artery (SFA) and the profunda femoris artery (PFA). (FIGURE 1) This bifurcation is usually at or below the bottom of the femoral head but, in approximately 25% of patients, occurs above this point; it is rarely opposite or above the ligament and occasionally more than 5 cm below the ligament. The PFA is at first lateral, then goes behind the SFA and ends at the lower third of the thigh in a small branch; the SFA ends at the junction of the middle with the lower third of the thigh, where it goes through the adductor canal (Hunter’s canal) and becomes the popliteal artery 2-4.
– Puncture of the femoral artery in routine cases
After palpation of the femoral arterial pulse, within the inguinal crease, an area around this point (about 10 cm in diameter) is identified and made sterile by painting with a povidone-iodine solution; the patient is covered from neck to feet, the sterile inguinal area being exposed. Both groins are routinely prepared, but the right one is usually used, because it’s close to the side of the operator. Selection of CFA puncture location is important to obtain optimal access and to avoid vascular complications. Indeed, it is well established that “high” puncture (above the ligament and above the centerline of the femoral head) is associated with increased risk of retroperitoneal hemorrhage and that “low” puncture (below the bottom of the femoral head, into the femoral bifurcation vessels) is associated with increased risk of haematoma, pseudoaneurysm and arteriovenous fistula. The ideal site of CFA puncture warranting safer access-site haemostasis may be assessed by fluoroscopy and is located below the femoral head centerline and relatively high within the lower inner quadrant of the femoral head (FIGURE 1). Such site is usually located 1-2 cm below the inguinal crease and is also the point of maximal arterial pulsation. As a consequence, many expert operators do not use to assess the optimal puncture site by fluoroscopy routinely. Nevertheless, the possibility to use a fluoroscopy-guided access (FIGURE 2) should strongly be considered during the learning curve and anytime the patient’s abdomen conformation suggests a possible displacement of the inguinal crease (like in obese patients), when a stent has been previously implanted in the ostial superficial femoral artery or when large sheaths should be inserted.
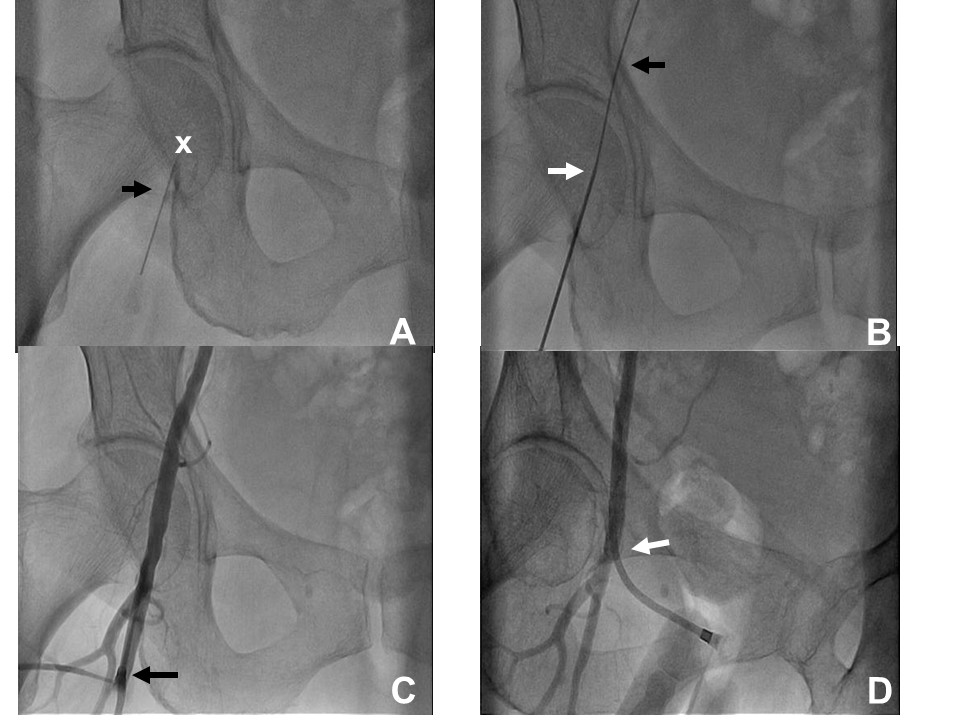
Figure 2
Once the location of CFA puncture is selected, local anesthesia is obtained by intradermal 1 or 2% lidocaine administration (10 to 15 ml) and the CFA is sticked at 45° angle with a 18-gauge open needle. As soon as the needle has been inserted within the artery lumen, the arterial blood backflow becomes evident and a 0.035- or 0.038-inch J wire is advanced through the needle into the vessel. In case of difficulty in advancing the wire beyond the tip of the needle, it is possible to exert a slight depression or to draw back the needle to improve the coaxiality between needle and artery. If there is no or poor backflow or if the wire cannot advance, the needle should be removed and repuncture should be attempted after manual compression. If the difficulty in advancing the wire is after several cm, it should be avoided to push it and fluoroscopy can be performed to assess the orientation of the wire’s tip. If the wire’s tip is not correctly oriented and subintimal track is suspected, the wire should be slowly removed. If the wire’s tip is correctly oriented, the sheath or its dilator should be advanced carefully over the wire (keeping it firmly in site) and then used for angiography after wire removal to identify tortuosity, stenosis or dissection.
If the careful advancement of the guidewire is optimal as far as the level of the diaphragm, the needle is removed and an introducing vascular sheath (with a backbleed valve and sidearm tubing) of appropriate size is placed over the guidewire.
Once the sheath has been inserted, the sheath’s dilator is removed and diagnostic or guide catheters may be inserted over the guide of an angiographic 0.035- or 0.038-inch 145-cm J guidewire.
– Techniques for specific settings
There are specific settings in which enhanced attention and dedicated strategies are needed to increase the safety of transfemoral procedures. For example, a suboptimal introduction site for femoral sheath, although unadvisable, may be acceptable during a diagnostic procedure with low or absent anticoagulation and immediate haemostasis but may result in catastrophic complications after an interventional procedure with adjunctive antiplatelet therapies, profound anticoagulation and deferred sheath removal. Thus, anytime incorrect entry location is suspected, before administering anticoagulation or planning the sheath removal, the location of sheath’s entry can be ascertained by performing retrograde femoral angiography through the sheath to identify the inferior bend of the inferior epigastric artery (as a landmark of the inguinal ligament), and the femoral bifurcation. Femoral angiography is also advisable on routine bases when the selection of femoral closure device is considered as correct entry site, adequate vessel size and absence of pronounced atherosclerotic disease are required for safe application.
Another setting requiring dedication is represented by the femoral artery puncture during procedures requiring very large sheaths. Intra-aortic balloon pump, cardiac assist devices and aortic valve interventions are increasingly applied in very fragile patients with complex vascular anatomies which may not tolerate access related complications. When more than arterial access is required for the procedure, iliac-femoral antegrade angiography may be performed from a different approach (radial artery or contralateral femoral artery) to select the best access site for bulky device insertion and to verify the presence of suitable arterial conduits. To ensure perfect arterial stick site in complex anatomies, the road-mapping tool may be easily used for an angiography-guided arterial puncture technique (FIGURE 3). Procedures with bulky devices are also associated with failure of haemostatic devices so that the achievement of post-procedural haemostasis may be checked by antegrade angiography obtained at the end of procedure by an other access site.
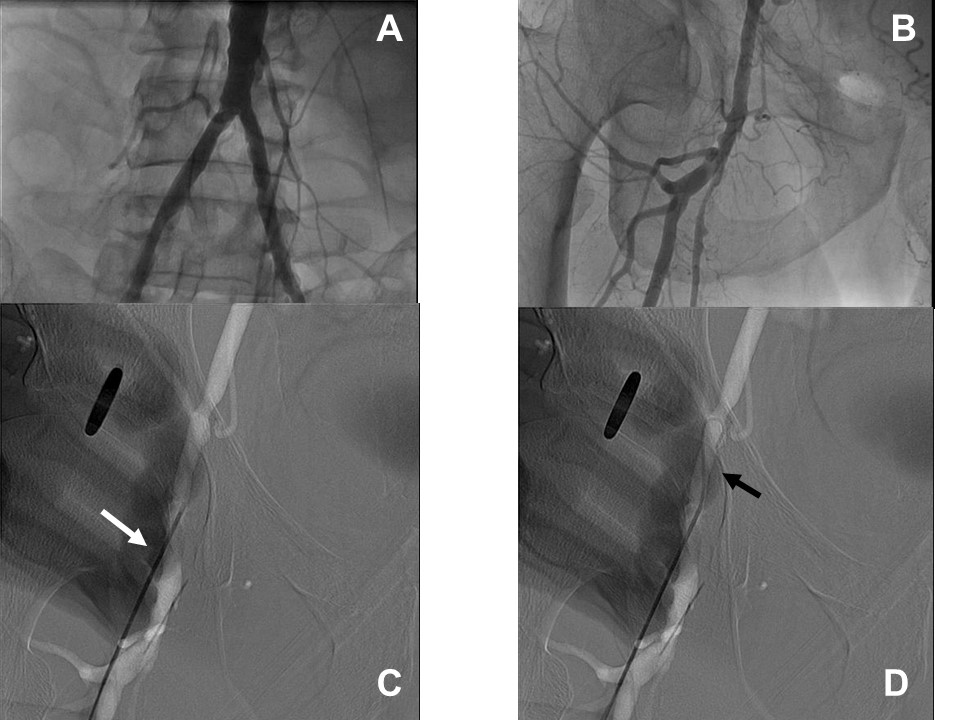
Figure 3